If you’ve ever heard someone say, “They had to rush to the Blood Bank,” or “The Blood Bank came to our school,” you’re not alone. The term “Blood Bank” is widely used — often as shorthand for an entire system of blood donation. But what exactly is a blood bank? Is it a place? A process? A part of a bigger organisation? The short answer is: yes, all of the above — and more. Let’s unpack the concept, function, and importance of blood banks in the life-saving world of blood donation.
How a Blood Bank Fits into a Blood Service
Here’s where some public confusion often arises. A blood bank is just one part of a much larger operation called a blood service.
A blood service, like the Western Cape Blood Service, oversees the entire journey:
- Donor recruitment and education
- Blood collection – at mobile clinics and blood donation centres
- Testing, processing, and storage
- Distribution to blood banks in hospitals
- Monitoring blood supply levels across the region
So, when people casually refer to the whole blood service as “The Blood Bank,” they’re not wrong, but they’re only naming one link in the chain.
The Big Picture: Blood Donation and Transfusion
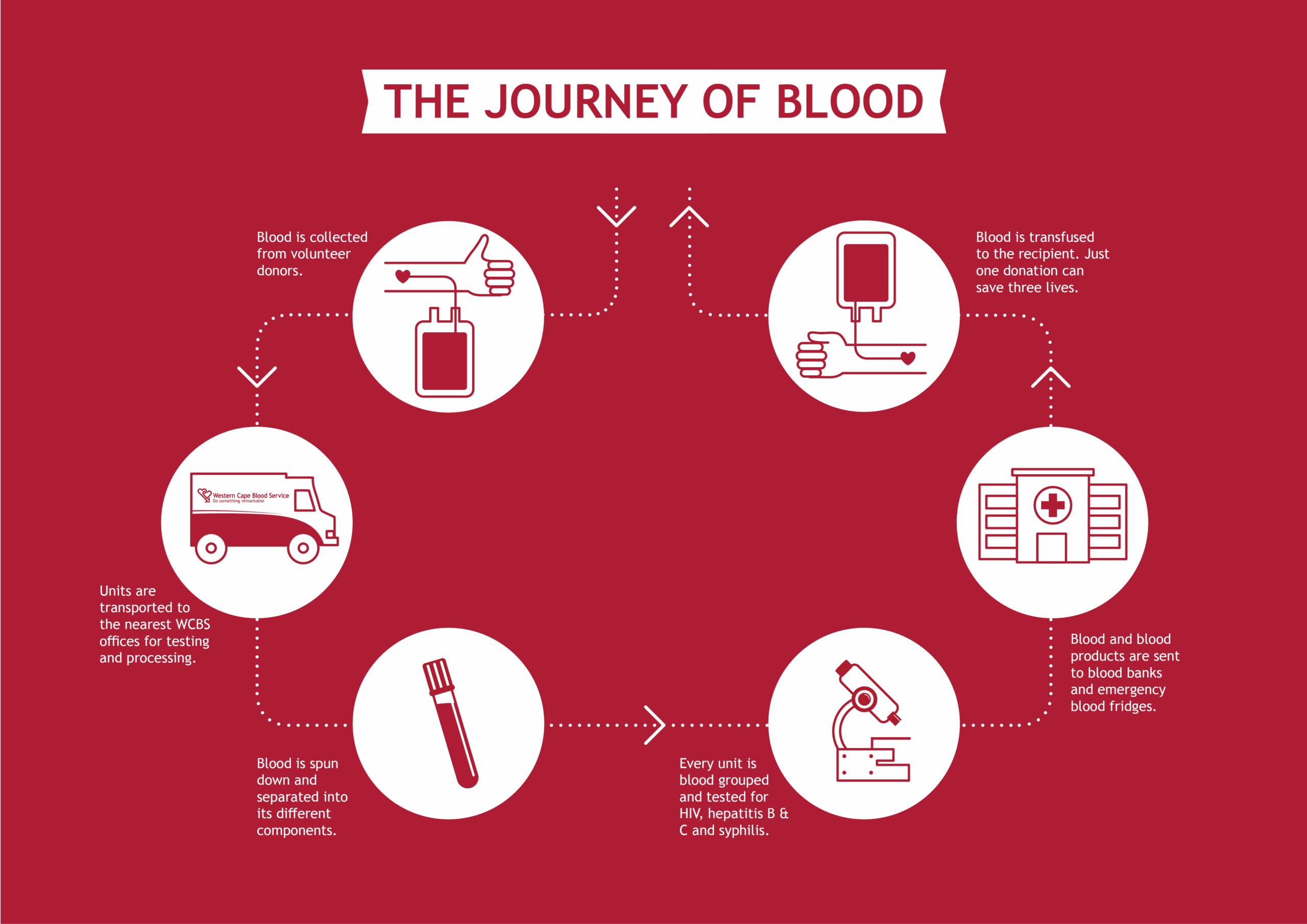
Before diving into what a blood bank is, it helps to understand the journey of a blood donation. When someone donates blood, that unit of blood doesn’t go directly into a patient’s arm. It first enters a complex, carefully regulated system that ensures safety, efficiency, and access to those who need it most. This system includes blood collection teams, laboratories, transport logistics, and yes — blood banks. In short, blood banks are the silent guardians at the end of the chain between donation and transfusion.
Let’s unpack it even further. Blood donors donate blood voluntarily at various blood donation clinics across the province. After the donation, the units are transported to the nearest Western Cape Blood Service offices for testing and processing. Each unit of blood undergoes a series of tests to ensure the safest blood possible. Each unit of blood is tested for HIV 1, HIV 2, hepatitis B & C, syphilis, and blood group (ABO and Rh factor).
Blood is separated into its various key components, such as
- Red Blood Cells (RBCs): used for trauma, surgery, anaemia
- Plasma: used for burn victims, bleeding disorders, and immune conditions
- Platelets: critical for cancer patients and people with clotting issues
This means one donor can save up to three lives, depending on the patient’s specific needs.
So, What Is a Blood Bank?
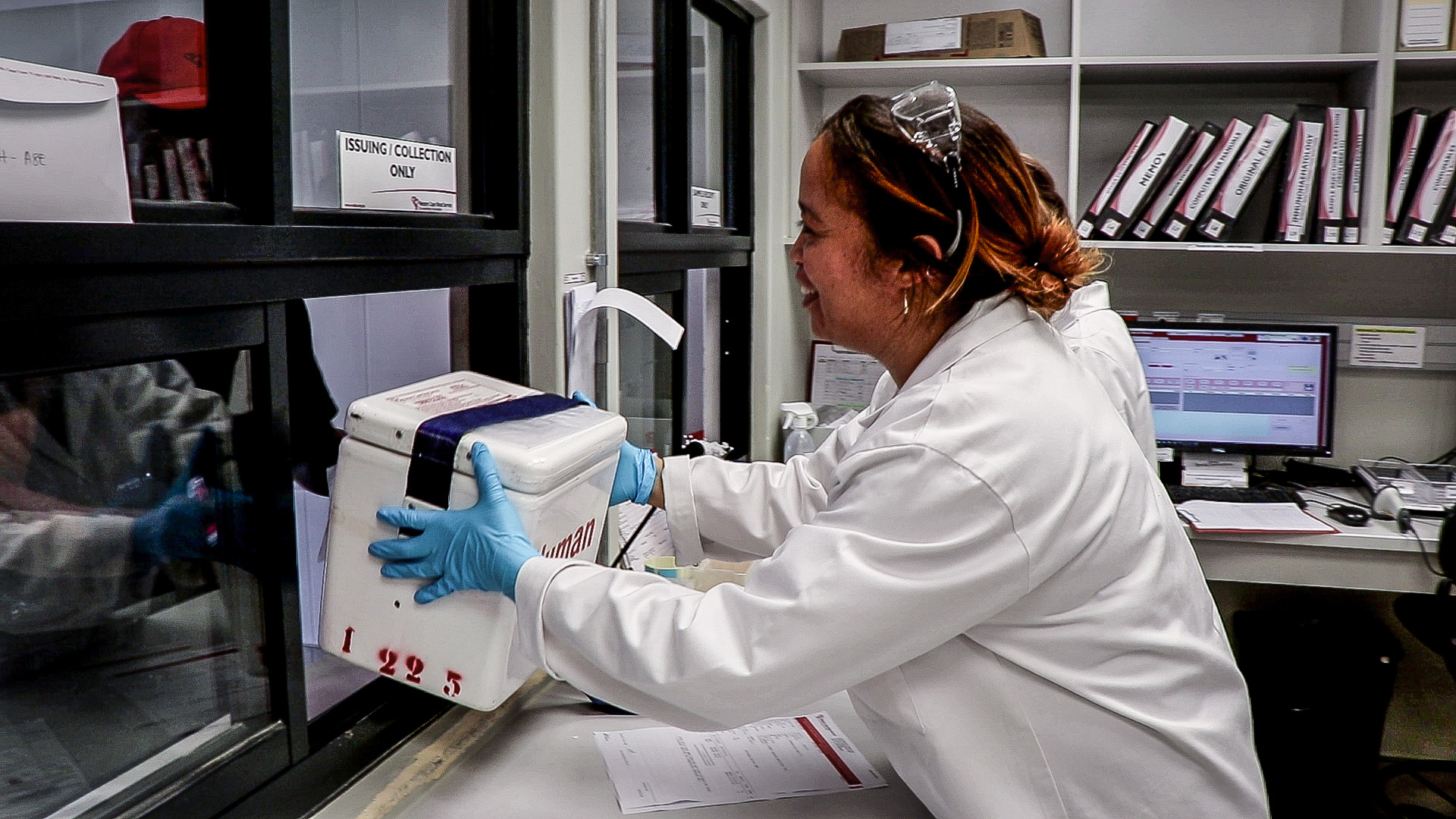
You can think of a blood bank as a laboratory, storage facility and pharmacy for blood products all in one. The primary role of the blood bank is to process patient samples in order to supply safe and compatible blood products to patients in need, while also performing supportive tests for other therapies such as solid organ transplants and obstetric care.
Here’s a Breakdown of What Happens in a Typical Blood Bank
When a patient’s request form and sample are received at the blood bank, the blood bank will check to make sure everything is completed correctly and is acceptable for testing.
Next, the patient will be registered in the system, and any historic transfusion testing records will be linked, if present, before the sample is prepared for testing.
For the majority of patients requiring red blood cells, routine testing involves three broad steps: ABO and Rh determination, antibody screening and compatibility testing.
ABO and Rh Determination
The first step is ABO and Rh determination. This is done in the same way as the ABO and Rh are determined for blood donors. Imagine the ABO and Rh antigens like individual shapes in a broader pattern. Your immune system recognises these patterns to detect foreign objects and eliminate them.
The good news is that, to your immune system, red blood cells from different individuals look similar enough that it will very rarely recognise or react to shapes absent from your own pattern unless it has already formed an antibody to highlight that shape.
While there are about 366 recognised blood group antigens, the ABO and Rh antigens are the most important antigens to match for most patients.
Antibody Screening
So, when do the rest of the 366 antigens come into play?
As mentioned above, ABO and Rh are the most important antigens to match for most patients.
During transfusion, organ transplants or pregnancy, a patient’s immune system is exposed to red blood cells other than its own. When this occurs, the immune system will sometimes form antibodies to any antigens that it does not recognise. It is these antibodies that can, in turn, trigger an immune response when the antigen is re-encountered.
To prevent an antibody from sneaking past, a screening test is done to detect the presence of any unexpected antibodies which may affect product selection.

Compatibility Testing
To ensure maximum patient safety, a compatibility test or “crossmatch” is performed to ensure that the unit is compatible. This is achieved by combining the patient’s plasma with red blood cells from a donor. If no reaction occurs, the unit is compatible. The crossmatch serves as a final step to ensure that the patient’s immune system will not attack the donor cells. Once a unit has passed the crossmatch test, the unit will be issued to the ward for transfusion.

Emergency Blood
The process above can take anywhere from 45 minutes to 2 hours, or even several days, if you have an extremely rare blood group. But what if you need blood NOW?
The WCBS also supplies 510 units of blood spread across 105 emergency blood banks and cardiac fridges situated at hospitals across the Western Cape.
These fridges contain strictly group O blood for use in emergencies when immediate transfusion is required. While blood products should ideally be crossmatched before transfusion, group O emergency blood allow maximum possible patient safety in the absence of a compatibility test. These group O emergency blood bags are replaced every three weeks to ensure that they do not expire.
Custodians of The Blood Supply
As the last link in the chain between donor and patient, the blood banks are responsible for maintaining the storage and preservation of a large portion of the total blood supply.
Frozen products, such as plasma, can be stored for over a year, while red cells are kept for 42 days, and platelet products are kept for five days. To ensure that no products expire before they are used, each blood bank keeps a supply to meet the demands of the hospitals it serves. This involves coordinating with the WCBS Processing and Inventory Control departments to ensure that products are available in sufficient quantities to meet patient needs while avoiding the expiry of unused products.
And There You Have It, Blood Banks in a Nutshell!
You can find our blood banks at the following sites:
- Groote Schuur Hospital
- Tygerberg Hospital
- Red Cross War Memorial Children’s Hospital
- Khayelitsha Hospital
- Mediclinic Vergelegen
- Paarl Hospital
- Worcester Blood Bank at our offices
- George Blood Bank at our offices.
Next time you hear someone mention “The Blood Bank”, you’ll know it’s not just a room full of fridges or a phrase tossed around in hospital dramas. It’s a vital part in a carefully orchestrated system — staffed by skilled professionals, guided by science, and fuelled by community generosity. Whether you’re a donor, a healthcare worker, or simply someone who might one day need blood, it’s reassuring to know that behind every bag of blood is a network of people and processes working around the clock to make sure the right product reaches the right patient at the right time.





