By Hayley Alie
The theme of this year’s World Patient Safety Day focused on “Medication Safety”. The Western Cape Blood Service (WCBS) uses a multilayered approach to ensure we can consistently provide safe blood products to our patient population.
According to the Standards of Practice for Blood Services in South Africa, WCBS follows strict guidelines pertaining to:
- Protection of the recipient (see standard TR 51-01) through very careful donor assessment to reduce the risk of transfusion transmissible disease. This is performed through completion of a detailed self-exclusion questionnaire and confidential interview of donors by the clinic staff.
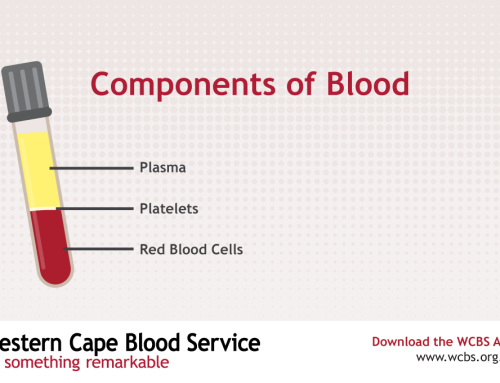
- Mandatory donation testing (see standard TR 37-01), quality control and visual inspection of blood components. Testing includes screening for specific infections through serological and/or nucleic acid techniques (NAT) for HIV-1/2, hepatitis B and C, and syphilis, as well as ABO and Rh grouping, allo-agglutinin titre and irregular antibodies. Only units that have passed all tests are labelled and distributed to blood banks for transfusion and compatibility testing. In the event that a donor’s subsequent blood donation is found positive for an infectious agent, a look-back investigation is conducted to identify and inform recipients about the risk of infection from the index donation. Blood components undergo routine visual checks for clots, haemolysis and any other abnormal appearances. Under exceptional circumstances, blood components may need to be issued when they do not conform to all mandatory donation testing requirements; this will be done at the discretion of the Medical Director and via documented notification to the requesting clinician.
- Processing of blood products (see standard TR 38-01) – The transportation and storage of blood donations and processed blood products is performed under strict cold chain management principles. The blood components are stored in sterile containers and sterile docking using a validated connecting device is performed when required. Each container is labelled with the donation number and batch number (for pooled products), so as to link it to the donor source for audit purposes. The container is also labeled with the product name, date and time bled, and expiry date and time.
- Compatibility testing and transfusion of blood products (see standard TR 39-01) – The blood request form and sample must be accurately labelled and the sample must be viable (less than 48 hours old) for it to be accepted in the blood bank. The minimum labelling information should include the hospital name and ward, patient’s first name and surname, date of birth, hospital number, primary diagnosis, date and time when the sample was drawn, name and signature of the phlebotomist, the requesting clinician’s name and their practice number (applicable for the private sector). If the patient has had a previous transfusion, the current blood grouping information will be compared to prior orders to confirm these results. Please note that inaccurately labelled request forms or cross-match samples will be discarded and new ones will be requested, to exclude the risk of patient misidentification. Where red cell components are requested, the blood bank will perform a compatibility test (called a ‘cross-match’) between the donor red cells and patient’s plasma prior to issuing the product. Where platelet and plasma products are needed, the bank will preferably select ABO compatible packs. Low titre ABO incompatible platelet and plasma products may be selected provided they do not contain significant amounts of red cells. Each suitably matched blood component will be labelled with the patient information and interpretation of the compatibility tests. The pack will be tied into the blood hamper to ensure its integrity, and the cold chain is maintained during transfer to the hospital and prior to commencement of the transfusion. An issue document that contains the patient and blood pack information will be provided with the blood hamper, and the hamper will be labelled with the patient name, hospital name and ward. In the event of a suspected adverse transfusion event, the transfusion should be stopped immediately and intravenous access maintained with normal saline. The event must be reported to the blood bank who will require a completed adverse event report form, all used and unused blood bags and a post-transfusion blood sample from the patient for investigation and prior to the re-commencement of further transfusions. A priority for the blood bank is to ensure that the right blood product is issued for the right patient at the right time. To this end, the person who collects the blood products from blood bank must present a visible means of patient identification ie. name, surname, date of birth and ID number.